Re Ian Bremmer 'Could third-party candidates upend the 2024 US election?' 3 April The current political movement in the USA…
Canada Healthcare
Written by Diana Thebaud Nicholson // June 22, 2015 // Canada, Health & Health care // Comments Off on Canada Healthcare
 Report of the Advisory Panel on Healthcare Innovation
Report of the Advisory Panel on Healthcare Innovation
Canadians working at all levels of healthcare observed that innovations of proven worth were not being scaled up and spread across the nation. For their part, entrepreneurs asked why it was harder to penetrate the Canadian healthcare market than to sell their ideas, products, and services abroad. While the Panel did hear complaints about the levels of funding available for healthcare, a surprising number of stakeholders echoed the growing public sentiment that a lack of operating dollars was not the primary problem.
On the positive side, as already indicated, there was an extraordinary consistency of resolve that real change in healthcare was greatly overdue. Front-line healthcare leaders, policymakers, and other stakeholders across the country were utterly consistent in this regard. While no one offered up a simple recipe for an excellent healthcare system, many themes recurred. (July 2015)
22 June
André Picard: In pursuit of ‘superhospitals,’ the public interest came last
On the weekend, the McGill University Health Centre celebrated the inauguration of its “Glen site,” a spanking new 500-bed hospital.
Normand Rinfret, president and chief executive of the MUHC, hailed the facility as a “shining icon for Montreal, for Quebec and for Canada.” He also thanked those who envisaged, designed, planned and managed the project and carried out the construction – and he did so with a straight face.
As hospitals go, it’s nice, especially compared with the decrepit, crumbling institutions it’s replacing, but it’s hardly iconic. It also comes with a whole of lot of baggage that can’t be conveniently overlooked.
The MUHC saga is a shameful example of the worst of petty politics and spineless policy-making, a two-decade-long debacle featuring corruption, bribery, petty politics and incompetence on a scale rarely seen in Canada.
 So, everyone paid $5 to walk to the MUHC and enjoy a fiesta while the PPP is charging the volunteer organizations who raise money for the hospital $60K p/a rent? And parking fees are almost $50 per day? I think there is something VERY wrong with this picture.
So, everyone paid $5 to walk to the MUHC and enjoy a fiesta while the PPP is charging the volunteer organizations who raise money for the hospital $60K p/a rent? And parking fees are almost $50 per day? I think there is something VERY wrong with this picture.
17-18 June
McGill University takes hit to prestige as medical school put on probation
(Globe & Mail) The Canadian and U.S. bodies responsible for accrediting medical faculties across the continent inspected the undergraduate program at the university this year and cited inadequacies in two dozen areas.
In a letter to faculty and students, [The dean of medicine, David Eidelman] said the university has 18 to 24 months to “demonstrate significant progress” on the problems authorities identified.
The flaws include concerns over students’ learning experiences and the quality of instruction in women’s health. … The U.S. Liaison Committee for Medical Education makes routine visits to faculties every eight years along with the Committee on Accreditation of Canadian Medical Schools. A joint team visited McGill in February and found 24 out of a total of 132 criteria lacking. McGill medical students’ concerns contributed to faculty probation — An independent student report that raised concerns about overwork and uneven supervision was one of the factors that contributed to McGill University’s faculty of medicine being placed on probation this week.
11 June
Montreal Chest Hospital says goodbye to historic building, joins Glen family
(Montreal Gazette) the hospital’s in-patients and those using it for 25,000 outpatient visits a year will benefit from a full complement of radiology equipment that it doesn’t have at its current site, two “beautiful” bronchoscopy suites and a better facility for a specialized form of bronchoscopy known as EBUS (endobronchial ultrasound) which is done increasingly often to diagnose lung cancer, infections, and other diseases causing enlarged lymph nodes in the chest.
The hospital will now also have access to all kinds of specialists for diabetes, heart disease and neurological disorders that it didn’t have on St-Urbain St. and which Olivenstein said will improve care for patients. It will have upgraded facilities for more pleural procedures (which tests the membrane surrounding the lungs), a state-of-the-art sleep disorder breathing lab and a pristine day hospital with 11 cubicles outfitted with comfy armchairs for people who don’t need to be admitted but require some intervention.
8 June
André Picard: A challenge for new doctors: Focus on the patient, not just the symptoms
(Globe & Mail) Shortly, you will be taking the Hippocratic oath. You’ve probably all heard that it says: “First do no harm.” It doesn’t actually – that’s just bad media reporting.
But it does say a lot of important things. I think the line that matters most in the oath is this: “Whatsoever house I may enter, my visit shall be for the convenience and advantage of the patient.”
Sadly, too many physicians fail to honour that part of the pledge.
We have built a sickness care system rather than a health system. We have designed that system for the convenience of practitioners, not patients.
Modern medicine has become so specialized that many physicians treat specific syndromes and body parts, and the patient herself gets lost in the process. We have filled our temples of medicine with such bedazzling high-tech tools that we’ve forgotten that we should treat people where they live.
In our desire to cure, we over-treat.
We fail too often to say the three most important words in medicine: I don’t know. We see death as a failure, instead of aspiring to make patients comfortable and at peace at end of life.
In our unrelenting quest for efficiency and measurement, we too often lose sight of what really matters. The patient.
25 May
Quebec family doctors won’t have to meet patient quotas
Bill 20 quota system won’t be enforced on general practitioners, as long as they meet 2017 deadline
(CBC) Quebec Health Minister Gaétan Barrette has made a deal with the province’s federation of general practitioners in an effort to improve access to family doctors.
Barrette will drop the idea of imposing a patient quota, but doctors will have to find a way to make sure 85 per cent of Quebecers have a family physician by the end of 2017.
 24 May
24 May
Recap: Children’s Hospital completes big move
As of 5 a.m. Sunday, the Montreal Children’s Hospital on Tupper St. has closed after treating thousands of kids at that address since 1956.
At that same hour, the emergency room of the new home of the Montreal Children’s opened at the Glen site of the McGill University Health Centre in Notre-Dame-de-Grâce.
Starting at 7 a.m., medical staff and Urgences-Santé paramedics were transporting pediatric patients — including premature babies — from the old location to the new Children’s Hospital.
The massive undertaking involving 19 ambulances, 675 staff and 60 volunteers had been completed by 11 a.m.
13 May
Dr. Mark Roper: Quebec is managing a first-rate medical system with second-rate data
Inevitably, the Health Ministry must rectify its method or face a worsening health crisis in central Montreal and oversupply in other areas. This will take political courage, as the regions that benefit from this mismanagement outweigh the regions that suffer from it. The only other alternative would be to force patients to see doctors in their home communities, a clear breach of the portability clause of the Canada Health Act.
(Montreal Gazette) In a health system that allows portability of health-care services from one region to another, areas that attract citizens for work, studies or play will naturally have more of their doctors being used by outside populations. And given that doctors’ offices are often located near major hospitals, areas with such hospitals might appear to be over-served, even if many of those doctors’ patients come from outside the neighbourhood. RLS DLM [Réseau local de service De la Montagne] has 384 family doctors practicing in the area, but, proportionally speaking, residents of that territory use the services of only 160 — well below the provincial average of 207 for a similar population. Patients from Cavendish (the territory of the N.D.G. and René-Cassin CLSCs) used 45.8 full-time family doctors in RLS DLM; from the South Shore, 32.3; from St-Laurent, 22.5; from the West Island, 22; from Laval, 18.9 and from Verdun, 8. The remainder came from other areas.
Specialists’ numbers are similarly affected.
Despite the availability of this data, the health ministry continues to use the number of doctors working in an area as the indicator of access that determines their distribution of doctors, instead of area residents’ actual use of services. This year, six of the 12 Montreal regions will have a net loss of family doctors after predicted retirements are taken into account. RLS DLM will suffer most, with a net loss of six, as it has the last four years and will continue to do in the future if policy does not change.
12 May
André Picard: Canada will have a national dementia strategy – eventually
Bill C-356, an Act Respecting a National Strategy for Dementia, was defeated last week in the House of Commons by the razor-thin margin of 140-139 NDP member Claude Gravelle sponsored the bill after watching his father struggle to care for his spouse, who was suffering from dementia. Like many people thrust into the role of caregiver for a loved one with dementia, the senior Mr. Gravelle soon realized that services are disjointed, help is difficult to come by and being a family caregiver 24/7 can prove costly – emotionally, physically and financially.
That we need a dementia strategy is a no-brainer – medically, economically and politically.
So why did Mr. Gravelle’s private member’s bill go down to defeat?
It’s all about political strategizing trumping sound public policy. Make no mistake, there is going to be a national dementia strategy. This is too important an issue for seniors – who vote in large numbers – for it to be ignored.The bill was defeated because the Conservative government wants to act on its terms, not have its hand forced by the opposition New Democrats. Bill C-356 called on the government to initiate discussions with the provinces and territories within 30 days on creating a “comprehensive national plan” and create an advisory board to do the actual grunt work of drafting a strategy.
If there is one political position that the government of Stephen Harper clings to fiercely, it is that health is strictly a provincial responsibility.
Still, the bill came surprisingly close to becoming law. It is worth noting too that a number of Conservative backbenchers broke ranks and voted for the bill, because they know that, on the campaign trail, being portrayed as someone who opposes a dementia strategy is going to hurt.
7 May
Tory MP Joe Preston Changes Vote, Kills NDP Bill Calling For National Dementia Strategy
Preston said he felt he couldn’t support Bill C-356, the National Strategy for Dementia Act, because it would commit the government to spending public money — something private member’s bills cannot do.
As chair of the procedures and House affairs committee, which is responsible for private members’ business, Preston said he felt he needed to hold himself to a “higher standard.”
The bill was introduced by NDP MP Claude Gravelle, whose mother also lived with Alzheimer’s disease.
Bill for national dementia strategy defeated by one vote
And while Health Minister Rona Ambrose supports the idea of a strategy, she also voted against it.
“I do support what Mr. Gravelle is doing,” said Ambrose. “But we’re working with the provinces and territories on developing a national strategy. So I’d prefer to work with them collaboratively because they’re all very receptive and we’re already well on our way to working together.”
While Ambrose has committed to funding research, there is disappointment among those who hoped for legislation toward a pan-Canadian strategy.
19 March
Opinion: Will a new MUHC be a renewed MUHC?
By Dr. Sherif Emil, director of the division of Pediatric General and Thoracic Surgery at the Montreal Children’s Hospital of the McGill University Health Centre.
(Gazette Opinion) I have been increasingly disappointed by what has happened to the MUHC and McGill’s other affiliated teaching hospitals. Although superb medical care is delivered every day by hundreds of skilled and selfless professionals, an unfortunate culture of indifference has crept into the hospital environment. The patient is often seen as a burden, rather than the organization’s raison d’être. This is manifested hundreds of times daily — in the technician who uses foul language, in the clinic clerk who speaks rudely to patients, in the nurse whose every move is saturated with frustration, in the physician who belittles the patient’s concerns or never returns their messages, in the administrator who fails to listen to those in the trenches.
Wrong wiring, nurse shortage in new ORs could lead to delays at MUHC superhospital
The wiring of the new operating rooms at the MUHC’s $1.3-billion superhospital is not adequate to run a key piece of surgical equipment, the Montreal Gazette has learned.
The hospital is also facing a shortage of trained operating room nurses.
MUHC officials are rushing to fix the problems before the superhospital opens on April 26 in Notre-Dame-de-Grâce, but the number of elective surgeries could be affected during the first few months — causing increases in wait times, a staff member who works in the ORs said. “In practical terms, they won’t immediately be able to have the same number of planned surgeries.”
13 March
Tunnel linking MUHC Glen site to transit isn’t wheelchair accessible
A tunnel linking to the McGill University Health Centre superhospital with the Vendôme métro and train station will only be completed by June.
The Agence métropolitaine de transport and MUHC officials showed off the tunnel to a select group of reporters from Global Montreal on Friday. The 34-metre tunnel, which will cost about $1.6 million to build, doesn’t connect directly into the hospital, but rather to its parking lot.
6 February
Doctor-assisted suicide: 10 voices on Supreme Court ruling
Ban on doctor-aided suicide to be struck down in 12 months, unless government responds with new law
(CBC) Reaction was swift and polarized after the Supreme Court of Canada ruled unanimously Friday that competent adults with grievous and irremediable medical conditions have the right to ask a doctor to help them die. The National Divided reaction to assisted suicide — For some the Supreme Court’s decision brings great relief, but to others it raises an alarm
Top court’s ruling on assisted suicide leaves many questions for doctors
(Canada.com) Canada’s highest court has left many questions for some of the central players in any future assisted death scheme — the very doctors who will be asked to help put to death adults who have decided life is no longer worth living.
What is “grievous” suffering? Who defines it? What form of “physician-assisted death” would be permitted? Death by a lethal prescription the patient would take herself, or death by lethal injection? Would physicians opposed to medical aid in dying have the right to refuse to even refer a patient seeking assisted death to another doctor willing to perform it?
Maher: Physician-assisted dying is a decision too tough for politicians
The ruling is 68 pages of good thinking. The nine justices of the court have delivered a compassionate, wise and clear decision, establishing sensible rules allowing doctors to help patients who are “grievous and irremediably ill” to end their lives.
… the Supremes have suspended their ruling to give Parliament 12 months to make a new law. MPs should have done so already. … The top court has only stepped in because Parliament has not done so.
5 February
Unique 20-year Canadian study of aging nears goal of 50,000 participants
Every three years, 50,000 Canadians will spend an hour answering a flurry of questions about everything from their sleep habits to how often they play a musical instrument or sing in a choir. Many will give up a few more hours for physical tests to check their hearing, bone density and heart function, among other things.
They’re being tracked for 20 years as part of an unprecedented study of aging in Canada. The Canadian Longitudinal Study on Aging started recruiting people between the ages of 45 and 85 in 2011 and now has about 45,000 on board.
“We will be finished recruitment of our 50,000 people and we’ll have finished our baseline assessment on everybody in the early summer of this year,” said Christina Wolfson, co-principal investigator in the national study and a medical scientist at the Research Institute of the McGill University Health Centre. “So it’s taken quite awhile to recruit these people.”
The ultimate goal, according to the study, is to learn how to improve Canadians’ health through a better understanding of the aging process.
30 January
Premiers urge Ottawa to do more on infrastructure, seniors’ health care
The country’s premiers presented a united front on everything from infrastructure and seniors’ health care to the need to protect Canadians from terrorism as they held their winter gathering on Friday without Prime Minister Stephen Harper.
… One of those accomplishments was a consensus on the need for a national strategy on seniors’ health care. Both the Canadian Medical Association and the Canadian Nurses Association had urged the premiers to address the issue at the meeting, and they heeded the call. Trudeau, Wynne lambaste Harper for skipping another first ministers’ meeting
29 January
Canada needs a national seniors’ strategy
All levels of government are at risk of being overwhelmed by Canada’s growing senior population and the health system’s inability to meet their needs.
(Toronto Star Opinion) As Canada’s premiers prepare to gather in Ottawa on Jan. 30 to meet as the Council of the Federation, we would like to remind them why a national seniors’ strategy must be high on their agenda.
The Mental Health Commission of Canada reported last week that family caregivers in Canada are experiencing extreme stress.
Among those aged 15 and over who provide care to an immediate family member with a chronic condition, 16.5 per cent reported very high levels of stress. Some 35 per cent of the workforce is providing care to a relative or friend, accounting for an annual loss in productivity of $1.3 billion.
Statistics Canada reports that family caregivers contribute an estimated $5 billion of unpaid labour to the health-care system. As our country’s older population grows, the need for care will only multiply. Recent Nanos public opinion polls conducted for the Canadian Medical Association and the Canadian Nurses Association found that an overwhelming majority of Canadians want the federal parties to improve financial support to family caregivers and to make seniors’ care part of their election platforms.
The tumbling dollar and sagging oil prices may get the headlines from the Jan. 30 council meeting. The real story, however, is how our municipal, provincial and federal treasuries are at risk of being overwhelmed by Canada’s growing senior population and the health-care system’s inability to meet the demand.
23 January
Louise Penny speaks out about life after her husband’s dementia diagnosis
Quebec author chosen as spokeswoman for Alzheimer’s Awareness Month
2014
7 December
Should Canadian medicare include drug coverage?
(Globe editorial) Two Canadian think tanks weighed in this week on the same issue – the state of provincial drug plans for seniors – but came to dramatically different conclusions.
A C.D. Howe Institute study concluded that age-based drug plans, which pay for medications for those over 65, will face huge cost pressures as the ranks of seniors increase dramatically in the coming years. Currently a majority of the provinces have these kinds of plans. A better alternative, the report says, is to base coverage on income, so those with the least resources – whatever their age – will get their drugs paid for.
The Institute for Research on Public Policy’s report, on the other hand, says that replacing age-based drug benefits with those based on income – as British Columbia and some other provinces have done – is a mistake. The deductibles that are a feature of income-base plans can hurt many seniors and add costs to the system, it says. The IRPP study favours full and universal coverage of drug costs. Such plans, it says, could be financed with small income tax hikes. And dramatic savings could be achieved if the provinces and territories create a central agency to buy drugs, thus generating huge discounts from bulk purchases.
IRPP Study: Are Income-Based Public Drug Benefit Programs Fit for an Aging Population?
Medications prescribed outside a hospital setting are not covered by Canada’s medicare system. They are financed through a patchwork of private and public drug insurance plans that only provide coverage for select populations, leaving many Canadians with little or no coverage.
Up until the late 1990s, people 65 and older received universal, almost first-dollar public drug coverage in most provinces. But with population aging, the public liability associated with age entitlements has become a major concern for governments. Four provinces have discontinued their age-based programs, which covered most of the cost of medications for seniors, and -replaced them with income-based programs, which protect all residents against catastrophic drug costs. Other provinces have started to move or are considering moving in this direction.
Is this sound policy? Steven Morgan, Jamie Daw and Michael Law assess the performance of -income-based public drug plans against three key policy objectives: access, equity and efficiency. They review the theory and the evidence by comparing Ontario’s age-based and British Columbia’s income-based systems. They find that income-based plans perform poorly with respect to all of these objectives.
13 November
Anxiety may accelerate slide into Alzheimer’s
While the link between depression and Alzheimer’s is already well established, little research has been done on how anxiety may contribute to dementia. A new study by Baycrest’s Rotman Research Institute in Toronto, supported by the United States National Institutes of Health, used data from the Alzheimer’s Disease Neuroimaging Initiative, which documented changes in cognition, brain structure and mental health in 376 adults, ages 55 to 91, with mild cognitive impairment – the kind of memory problems that make people forget what they are about to say or why they went into a particular room.
Dr. Linda Mah, a psychiatrist at the University of Toronto and principal investigator on the study, explained that people with anxiety disorders have higher levels of the stress hormone cortisol, which has been shown to damage the hippocampus, a brain structure important for memory processing and emotion.
For people in their 30s and 40s, the study should serve as a “wake-up call,” she added. And for older patients, mindfulness-based stress reduction is being studied as a potential intervention. (It will be the focus of a researchers’ conference in Toronto in December.) Mah and colleagues were able to separate the effects of anxiety from those of clinical depression, since only patients with low depression scores were included in the study. At the onset, patients were able to function in everyday life, but suffered from memory problems that were mild but considered red flags: “This is not normal aging, but a prodrome [symptom] of Alzheimer’s,” Mah said.
In patients whose condition deteriorated into Alzheimer’s disease, magnetic resonance imaging (MRI) detected structural changes, including atrophy, in brain regions involved in creating memories as well as processing emotions.
Also of interest: New Alzheimer’s-related memory disorder identified
(Medical Press) A multi-institutional study has defined and established criteria for a new neurological disease closely resembling Alzheimer’s disease called primary age-related tauopathy (PART). Patients with PART develop cognitive impairment that can be indistinguishable from Alzheimer’s disease, but they lack amyloid plaques. Awareness of this neurological disease will help doctors diagnose and develop more effective treatments for patients with different types of memory impairment. … In the current study, investigators from the United States (including five from Sanders-Brown), Canada, Europe, and Japan came together to formalize criteria for diagnosing this new neurological disorder. The study establishes that PART is a primary tauopathy, a disease directly caused by the tau protein in tangles.
31 October
Canadian Visa Ban Issued To Residents Of Ebola-Stricken Countries
In a move that puts Canada at odds with the World Health Organization, the federal government said Friday it is suspending the issuance of visas for residents and nationals of countries with “widespread and persistent-intense transmission” of Ebola virus disease. As well, work on permanent residence applications for people from the affected countries is also being suspended. …
During SARS, the World Health Organization issued travel advisories directing people around the world to avoid places battling outbreaks. It is a tool the organization has never used again.
One of the places hit with a travel advisory was Toronto.
Two prominent members of Prime Minister Stephen Harper’s cabinet — Treasury Board Chairman Tony Clement and Foreign Affairs Minister John Baird — were then part of an Ontario government that roundly denounced the WHO for the travel advisory. … Clement, then Ontario’s health minister, led a delegation to Geneva — an extraordinary move, given that the WHO only deals with national governments — to demand the WHO rescind the travel advisory against Toronto.
CBC The National: The Sunday Panel with Margo Somerville, Jonathan Kay and John Moore (20:20) debate assisted suicide in light of forthcoming Supreme Court hearing on October 15. [Supreme Court to rule soon if assisted suicide is a human right]
18 October
Les millionnaires de la santé
(La Presse) Le Dr Barrette a contribué plus que n’importe qui à l’explosion des coûts de santé en négociant pour les médecins spécialistes des augmentations dont ils n’osaient pas rêver eux-mêmes. Une fois la job bien ficelée, il a empoché une grasse compensation de sortie et est entré en politique comme ministre pour «mettre de l’ordre dans le système». En gestionnaire lucide conscient des limites de ce système, il retrouve la mémoire et souligne la nécessité de se serrer la ceinture.
Pour éponger un déficit dont il a lui-même accru la gravité, il compte effectuer des coupes dramatiques, non pas dans le salaire exagéré des médecins, mais partout ailleurs. En fait, ces coupes serviront essentiellement à financer les augmentations de ses confrères, et ce n’est pas sa petite mise en scène gueularde où il fait passer pour un exploit l’étalement superficiel de salaires coulés dans le ciment qui gommera les effets récurrents de cette catastrophe. Comme comble de cynisme, c’est difficile de grimper plus haut.
6 October
No magic pill solutions in Rona Ambrose’s crusade against opioid
Yes, doctors need to prescribe fewer opioids. Many of them agree with Ms. Ambrose, including the CEO of the Royal College of Physicians and Surgeons of Canada. But doctors can’t just stop treating a patient’s chronic pain. They need alternatives. Long-term pain management without opioids requires education, counselling, lifestyle changes and repeat visits to the doctor. Hospitals need to be able to offer surgery more quickly to patients in pain, and they need to develop more modern, less invasive surgical procedures.
Harper Government Invests in National Initiative to Tackle Dementia
CIHR and partners launch the Canadian Consortium on Neurodegeneration in Aging a collaborative research program focused on tackling the challenge of dementia and other neurodegenerative illnesses
September 10, 2014 – Montreal, Quebec – Canadian Institutes of Health Research
The Honourable Rona Ambrose, Minister of Health, today announced the launch of the Canadian Consortium on Neurodegeneration in Aging (CCNA), a national initiative aimed at tackling the growing onset of dementia and related illnesses and improving the lives of Canadians with these illnesses, as well as their families and caregivers.
Led by Dr. Howard Chertkow, a cognitive neurologist and co-founder and director of the Jewish General Hospital / McGill Memory Clinic, the CCNA brings together 20 research teams and experts from across Canada to focus research on three themes:
delaying the onset of dementia and related illnesses
preventing these illnesses from occurring
improving the quality of life of Canadians living with these illnesses and their caregivers
The CCNA is supported with funding of $31.5M over five years from the Government of Canada through the Canadian Institutes of Health Research and a group of 13 partners from the public and private sectors, including the Alzheimer Society of Canada and Fonds de recherche du Québec – Santé. The CCNA researchers will also benefit from an additional $24M investment by a subset of the partners in Ontario and Quebec.
Minister Ambrose made the announcement ahead of the Canada-France Global Legacy Event to be held in Ottawa, September 11 and 12. The event will bring together 200 experts from G7 countries and focus on building global academic-industry partnerships and promoting innovation in dementia prevention, treatment and care.
The CCNA is headquartered in the Lady Davis Institute at the Jewish General Hospital.
McGill professor to head national research program into dementia
For neurologist Howard Chertkow, medicine’s hardest challenge is Alzheimer’s disease, given there is no way to prevent, cure or slow its progression.
On Wednesday, the professor of neurology at McGill University and director of the memory clinic at the Jewish General Hospital officially became scientific director of a national research program worth $31.5 million over five years — one of the largest of its kind — to tackle brain diseases associated with old age.
The initiative marks a growing urgency over the health, social and economic burden of dementia worldwide. In Canada alone an estimated 747,000 people were living with Alzheimer’s or other forms of dementia in 2011, a figure that’s expected to be a rising tide with the greying of the population to 1.4 million by 2031, costing the economy nearly $300 billion per year.
‘It’s not even known whether Alzheimer’s is one disease or many,’ Jewish General neurologist Howard Chertkow says
(Journal de Montréal) Vaste initiative pour lutter contre la démence Cette vaste initiative de recherche sera dirigée depuis Montréal par le Dr Howard Chertkow, éminent neurologue cognitif, cofondateur et directeur de la clinique de mémoire de l’Hôpital général juif. (CBC) National dementia research intitiative gets $31.5M federal funding Additional $24M coming from provinces
Ambrose will make another announcement on Thursday in Ottawa at the Canada-France Global Legacy Event, a two-day gathering of about 200 experts from G7 countries on dementia care and treatment, as well as ways of improving the lives of caregivers.
(Globe & Mail) Ottawa to fund research on dementia, other neurodegenerative diseases The federal government announced funding Wednesday for a national research program to look into dementia and other neurodegenerative diseases. The Canadian Consortium on Neurodegeneration in Aging will bring together 340 researchers who are part of 20 teams across Canada, Health Minister Rona Ambrose said.
(Mtl Gazette) Ottawa invests $31.5 million for dementia research
“Diana Nicholson, whose husband, David, is enrolled in Alzheimer’s therapy trial, said she is grateful to be part of this research family, which is also providing guidance on care at home.”
(CTV) Montreal chosen as battleground in fight against dementia
4 September
Claire Webster: Help is available for Alzheimer’s caregivers
2 May
The Big Move: Hospital transfer will be historic undertaking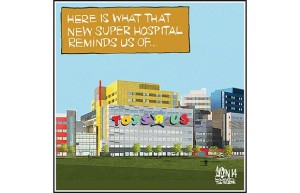
Shifting patients and staff from the Royal Victoria to new MUHC superhospital will be a massive and complex challenge
(Montreal Gazette) Imagine, if you will, that you’ll be riding in a helicopter on the morning of Sunday, April 26 next year — hovering over the city near the Scottish baronial towers of the Royal Victoria Hospital. What you’ll likely see on that date will no doubt present a unique image in not only Montreal’s history, but all of Canada’s.
From 6 a.m. that morning, you will glimpse a caravan of ambulances — dozens of them — transporting as many as 300 patients to the city’s first superhospital in Notre-Dame-de-Grâce. The patients will include, among many others, those recovering from heart surgery and the frail receiving palliative care in the last days of their lives.
Police will be escorting the ambulances or stopping traffic at intersections to wave them through. Two by two — patient and health-care worker — will be riding in each ambulance as it speeds to its final destination: the vast new hospital of the McGill University Health Centre. It’s an image so epic in scale that it’s not an exaggeration to suggest it recalls God’s creatures boarding Noah’s Ark.

28 April
The secret slang of hospitals: What doctors and nurses call patients behind their backs
In his new book, The Secret Language of Doctors, Dr. Brian Goldman reveals a veritable dictionary of verbal shorthand used by many physicians, nurses and other health professionals to discuss — and often diss — various types of patients and even their own colleagues.
Despite its title and contents, Goldman maintains the book isn’t meant to be just about the jargon that medical personnel trade amongst themselves.
“It’s a book about what the language reveals about the culture of modern medicine and what’s inside the heads and hearts of physicians and allied health professionals, but also the problems that they face, the challenges,” he says.
15 January
Canadian Institutes of Health research
Pot and Politics: Canada and the Marijuana Debate;
Montreal superhospitals may charge for overnight stay
Quebec health ministry will consider a sliding-scale formula based on patient income
(CBC) With the aim of reducing the risk of spreading infections, the new hospitals — one managed by the McGill University Health Centre network (MUHC) and the other managed by the Centre Hospitalier de l’Université de Montréal (CHUM) network — will only have private rooms, according to Radio-Canada’s program La Facture,
Quebec patients have traditionally had to pay extra fees for that level of privacy. At the Montreal General hospital, patients fork over $71 a night for a semi-private room and $141 for a fully private room
2013
7 December
The Guru and the Hackers
(CBC radio) This week on White Coat Black Art, Dr. Brian Goldman looks at the rocky relationship between health care and information technology.
Dr. Goldman and medical journalist Dr. Meera Dalal take us to Hacking Health Toronto. It’s a weekend-long hack-a-thon that connects health professionals with software designers, engineers, and computer visionaries. Their goal is to take an idea and turn it into a killer health-care app in just forty-eight hours.
26 September
Innovation in 3D printing and spinal bone grafts at Canada’s McGill University
A team led by McGill University’s Dr Michael H Weber, and Professor Jake Barralet, are developing a new technology with a 3D printer which seeks to create replicas of bone for spinal grafts..
The concept creates a bone-like replacement material in the exact shape of bone or bone segment which is to be removed.
The idea of 3-D printing is gaining ever increasing usage. Already becoming established in dentistry, surgeons and researchers like the McGill team are exploring new uses in bone grafting and medicinal targetted delivery. Although the basic principal is similar to use in dentistry, the McGill research is extremely more complex in materials, designs and application.
Professor Barralet, is developing new bio-ceramic based materials which mimic bone structures and which would promote actual bone to grow over the “scaffold” substrate. Because of the nature of the materials this promotes natural repair of damaged areas giving them back their original structure and strength.
Canadian doctor total at record high
Number of female doctors rose nearly 24%, male doctors increased 10%, CIHI says
(CBC) Canada had a record 75,142 doctors last year and they earned $328,000 gross on average, according to two new reports.
The annual reports on physician supply and payments for both general practitioners and specialists were released Thursday by the Canadian Institute for Health Information.
What’s more, the six-year trend of growth in the number of doctors outpacing population growth is expected to continue since data from medical schools indicate more students are graduating with MD degrees.
13 May
Steven Lewis and Terrence Sullivan: How to Bend the Cost Curve in Health Care
(IRPP Insight) Summary
— Whatever money is saved through short-term restraint will be lost in panicked spending down the road. That’s been the lesson of the past 20 years.
— The challenge is to bend the cost curve permanently while making the system perform better. What health value do we achieve for what we spend?
— Improving value for money will require governments, organizations and practitioners to leave their comfort zone of conventional practice.
29 January
Michel Kelly-Gagnon: New Prescription Drugs Are Worth the Cost
(HuffPost) We cannot deny the fact that the costs of prescription drugs have been increasing at a considerable rate over the last few decades. Prescription drugs spending as a share of all healthcare expenditures in Canada rose from 6.3 per cent in 1975 to 13.4 per cent in 2012. While total healthcare spending per capita has almost tripled during this period, per capita expenditures on prescription drugs have increased six-fold.
But should this trend be a source of concern? Not necessarily. Although costly in the short-term, new drugs tend to lower overall health spending in the long run, by reducing expenditures on other categories of medical care. Indeed, innovative pharmaceutical therapies have been, over the years, increasingly substituted for other, more costly types of medical treatments and surgeries that require hospitalization.
2012
22 November
a href=”http://www.grandchallenges.ca/stars-r3-grantee-announcement-en/”>Grand Challenges Canada: Funding for inventive health projects in developing countries
The government funded body awards $100,000 financial seed grants to innovators around the world, and will be looking for more ideas in the next few months.
Grand Challenges Canada announces 68 grants awarded to 17 innovators in Canada and 51 innovators in the developing world for their bold and creative ideas to tackle health conditions in poor countries. The projects were submitted in response to Stars in Global Health – Round 3, a program that supports exceptional innovators who have Bold Ideas with Big Impact in the area of global health, and who are based either in Canada or in low-income or lower-middle-income countries. The projects that received funding are summarized below, listed in alphabetical order by country. Click on the project links to read the project summary, watch a short video and download images.
30 September
Doctors, developers hacking their way to better healthcare
(CTV News) Software developers often use “hackathons” to brainstorm ideas with colleagues, especially to design games and create new social media tools. But a new grassroots organization is putting doctors and developers together to hack their way to solutions to health-care inefficiencies.
On a recent Wednesday evening in Toronto, a few dozen developers converged on Toronto General Hospital to discuss Hacking Health’s three-day hackathon in October. …
Co-founder Jeeshan Chowdhury, himself a PhD in health information systems and a third-year medical student at the University of Alberta, said the idea for Hacking Health came to him at a health conference in Montreal. He attended a discussion on health care innovation, which was led by a panel that didn’t know the first thing about technology, or software design and development. …
Hacking Health came together pretty quickly after Chowdhury joined forces with an executive in the eHealth sector, Luc Sirois.
17 August
Canadian research could lead to the elimination of hip and knee replacement surgery
(RCInet) Dr Nizar Mohamed of the University Health Network in Toronto has been looking in using stem cells to grow cartilage. If successful, the cartilage could replace damaged cartilage caused by arthritis in such areas as hip joints and knees. This has the potential to reduce the costly and invasive surgeries for replacement of hips and knees. Currently there are about 50-thousand such surgeries annually in Ontario alone. In the US its about a million such surgeries annually.
12 August
Stem cell cure for implants under research at Toronto hospital
31 July
Incoming head of Canadian Medical Association sees a ‘deeply demoralized’ medical profession
(Canada.com) The emergency physician at Stanton Territorial Hospital assumes the helm of the Canadian Medical Association in August, when more than 300 delegates gather in Yellowknife for the CMA’s 145th annual general council meeting.
[Dr. Anna] Reid will be the first CMA president from the Northwest Territories. It will also be the first time the annual meeting will be held in the Northwest Territories.
The assembly of what has been dubbed the “parliament of Canadian medicine” comes amid fresh warnings from Canada’s premiers that a new 10-year federal health accord will gut nearly $36 billion in funding to the provinces, resulting in less money for doctors, nurses and health care across the country.
Earlier this year outgoing CMA president Dr. John Haggie accused the Harper government of gnawing away at the country’s social safety net, warning that plans to raise the pension eligibility age to 67 would force low-income seniors to choose between buying groceries or buying medicine.
Reid says the profession has become “deeply demoralized” through the years because of a “top-down, this-is-what’s-going-to-happen” approach to local health planning and a federal government that seems to be distancing itself from health care.
26 July
Premiers forge own health-care path
(Globe & Mail) Canada’s premiers are taking the lead on health-care reform without direct leadership from Ottawa, a departure from the way the country’s cherished but increasingly expensive system has long been managed.
By acting alone, the premiers are answering Ottawa’s call to action. Late last year, Prime Minister Stephen Harper granted provinces more autonomy to reshape health care as Ottawa moves to end 50 years of using its funding power to coerce provinces to adopt national standards.
Mr. Harper essentially asked provinces, with some federal guidance, to do as they see fit in their own jurisdictions while inviting them to co-operate in establishing national benchmarks for delivering health services.
Premiers talk health care … at Halifax summit
(CBC) At the premiers meeting in Halifax today, the provincial leaders spent the morning talking about health care and said they want to use teams to better care for patients and save money by buying a few generic drugs in the next year.
The two ideas are some of the recommendations coming out of a six-month study led by the premiers of Saskatchewan and Prince Edward Island.
‘Co-ordinated approach’
Saskatchewan Premier Brad Wall says the federal government “stated pretty clearly by what they didn’t say and what they did say that they weren’t perhaps as interested in innovation as we’d like.”
The report contains a dozen main recommendations and broadly covers:
– How regions can stop poaching doctors and nurses from each other.
– How provinces can bulk buy some generic drugs to save money.
– How patients receive treatment – what kind of treatment, and from whom.
– Specifically, the report recommends that starting this fall, the provinces pick three to five generic drugs to be part of a bulk buying program to get better prices. The first group order is expected next spring.
– The report also recommends that provinces use new guidelines in treating heart disease and diabetes, address health human resources, and create a new website to better communicate about labour markets. And Wall suggested engaging front-line workers in how to save money on operations and capital, which he says has saved his province millions of dollars.
Premiers should also consider adapting best practices from the provinces that are effectively using health-care teams to better look after patients, according to the draft report. It quotes examples in Alberta, Ontario and Quebec, provinces where nurse practitioners do primary care.
20 July
Harper Government Supports Health Care Innovation
(Press Release) The Honourable Leona Aglukkaq, Minister of Health, visited with researchers at Lawson Health Research Institute (Lawson) today where she highlighted how Harper Government investments are helping strengthen healthcare across the country. Lawson is the research institute of London Health Sciences Centre (LHSC) and St. Joseph’s Health Care London. The Minister also toured research labs at LHSC’s Victoria Hospital.
12 July
Fraser Institute report claims thousands have left Canada for medical care
(Yahoo!) The right-leaning Fraser Institute is stirring the pot with a new report that claims that 46,169 Canadians left the country to get medical treatment elsewhere in 2011.
“In some cases, these patients needed to leave Canada due to a lack of available resources or a lack of appropriate procedure [or] technology,” Nadeem Esmail, the author notes in his report.
5 July
Common diabetes drug promotes development of brain stem cells
Researchers at The Hospital for Sick Children (SickKids) have found that metformin, a drug commonly used to treat Type II diabetes, can help trigger the pathway used to instruct stem cells in the brain to become neural (nerve) cells. Brain stem cells and the neural cells they generate play a role in the repair of the injured or degenerating brain. This study suggests a novel therapeutic approach to treating people with brain injuries or potentially even neurodegenerative diseases.
Dépression: les préjugés persistent au Québec
(La Presse) La dépression est toujours perçue de manière très négative au Québec. Près de la moitié de la population ne voterait pas pour un politicien atteint de la maladie ou n’engagerait pas une personne qui présente des symptômes de dépression, révèle un sondage interne du ministère de la Santé que La Presse a obtenu. L’étude montre aussi qu’une campagne publicitaire du gouvernement a été peu efficace pour éliminer les préjugés.
3 July
Ottawa backs down on refugee health-care cuts
(Toronto Star) Ottawa has backed down on its health-care cuts for resettled refugees on income support, but other asylum seekers are still not immune from the axe.
The federal government quietly amended information about the changes on its website late Friday, just before the cuts to the Interim Federal Health Program (IFHP) kicked in on the weekend.
As a result, impoverished refugees resettled to Canada through government and private sponsorships can still access hospital services, diagnostic and ambulance services, as well as supplementary health support such as wheelchairs, dental and vision care — equivalent to what is available to low-income Canadians.
Critics who fought staunchly against the cuts said Ottawa’s flip-flop indicates the government’s recognition of vulnerable refugees’ health-care needs.
18 June
(CBC) Federal cuts to refugee health care draw protests
10 June
The prime mover behind this wonderful acquisition has been our neighbor, Sandra Mavridakis on behalf of her son Emmanuel (see the embedded video)
Un premier appareil Lokomat au Québec
Des jeunes aux prises avec des déficiences motrices pourront bientôt réapprendre à marcher grâce à un appareil technologique de pointe.
D’ici la fin du mois de juillet, le centre de réadaptation Marie Enfant, à Montréal, recevra le tout premier «Lokomat» de la province, a appris La Presse. Ce robot aide les patients à marcher en soutenant leur corps, ce qui permet d’accélérer leur réadaptation.
Le robot, commandé des Pays-Bas vendredi dernier, coûtera au total près de 650 000$ au centre de réadaptation. L’achat est le fruit de six mois de financement provenant de deux fondations, soit celle du centre Marie Enfant – Mélio – et celle du CHU Sainte-Justine.
«En ce moment, il faut trois aides professionnelles pour qu’un patient puisse faire 10 minutes de marche assistée. Mais avec le Lokomat, il pourra faire une heure de marche assistée seul», explique Catherine Sevigny, directrice générale de la Fondation Mélio. En plus d’être plus efficace, le robot comptabilise les données, ce qui permet de mesurer l’évolution quotidienne des jeunes.
29 March
Budget 2012 misses mark on health leadership, says CHA
The Canadian Healthcare Association (CHA) notes that Budget 2012 reflects the government’s focus on creating jobs and economic growth for Canada. But when it comes to health system improvement, CHA asks, where is the federal leadership?
“Budget 2012 addresses a number of important health concerns,” said Pamela C. Fralick, President and CEO, Canadian Healthcare Association. “But, Canada will not have the world class health system it deserves with a piecemeal approach. Federal leadership is a necessary component of comprehensive health system improvement.”
CHA was pleased by announcements for an important network of mental health researchers focusing on depression and PTSD, genomics research, and research on interprofessional healthcare teams through McMaster University, and alternate sources for medical isotopes. While student loan forgiveness for doctors and nurses who work in rural and remote areas is welcome, CHA would like to see this extended to other health professions.
16 January
Quebec premier calls health-care funding formula ‘unacceptable’
Quebec Premier Jean Charest blasted on Monday Prime Minister Stephen Harper for refusing to explain to Canadians why he is slashing funds for medicare.
12 January
Provinces will be burdened by health-care costs: Kevin Page
The Conservative government’s decision to trim the growth in health-care funding will help ensure long-term fiscal sustainability of federal finances but will place a huge financial burden on the provinces, says Parliament’s spending watchdog.
Parliamentary Budget Officer Kevin Page released a report Thursday examining the projected financial health of the provincial and federal governments, following Ottawa’s announcement of a new 10-year health funding agreement that will slowly scale back the growth in health transfers.
2011
20 December
Top 10 health stories of 2011: food chemicals, vitamin D and brain waves
Article on how EEGs can measure awareness of vegetative patients takes top spot
11 November
Veterans’ health concerns demand more research funding
(CBC) Canadian military veterans and veteran research groups are calling for a funding increase to assist returning soldiers who struggle with their mental and physical health.The Canadian Institute for Military and Veteran Health Research focuses on both the mental and physical health of new veterans. It officially launched this fall in Kingston, Ont.
15 February
Diabetes discovery brings out hospital’s entrepreneurial side
(Globe & Mail) Tuesday’s agreement between Sanofi-Aventis and Sunnybrook Health Sciences Centre on a wound-healing molecule demonstrates how entrepreneurial hospitals can become when the very sustainability of medicare is in question.
20 January
Canada’s North frozen out of doctor supply
In southern Canada, one doctor cares for an average of 438 people, but in the country’s northern regions, one physician is responsible for the health of as many as 3,333 people, according to a new report from the Conference Board of Canada.
The most acute shortages are in northern Saskatchewan, Nunavut and northern Newfoundland and Labrador, the latest report from the organization’s Centre for the North research institute finds.
12 January
Private rooms save lives and money
(The Gazette editorial) the McGill University Health Centre and the Centre hospitalier de l’Universite de Montreal will have a total of 1,272 private patient rooms, including those in the intensive-care units.
There’s no time to waste getting those rooms operational. For years now, Quebec’s crowded and under-maintained hospitals have been the breeding grounds for tenacious hospital-acquired infections like C. difficile. As a new study this week shows, private rooms can go a long way to preventing those infections.
(Reuters Health) – Intensive care unit (ICU) patients placed in private rooms may pick up less than half as many infections as those in rooms with multiple beds, hints a new Canadian study. Read more
2010
20 December
French superhospital facing higher costs, more delays
(CTV) Construction on the McGill University Superhospital, as well as the new Montreal Children’s and Shriners Hospitals, began this past summer in the Glen Yards.
But the long-awaited French language CHUM hospital, first proposed in the mid-1990s and projected to be completed in 2003, is now facing even more delays and a massive $300 million increase in its cost estimate.
22 September
Quebec is right to drop its user-fee plan
What was going to be called a health deductible would have charged Quebeckers for the “consumption of health-care services” and was projected to bring in $500-million as of 2013-14. Charges seemed likely for doctor’s office or hospital visits.
16 September
Keith Martin, MD; Member of Parliament, Esquimalt-Juan de Fuca, B.C., Liberal Party of Canada
Our Health-Care System Needs Urgent Care
Canadians must embrace the resources locked within the private sector if we are going to have a sustainable health care system. These are the findings of the just-released Organization for Economic Co-operation and Development report, which thoroughly debunks the myth that Canada has the best health-care system in the world.
13 September
Universal pharmacare touted as way to save billions
(Globe & Mail) New study dismisses out-of-hand the notion that a public drug plan is unaffordable
The report argues that Canada’s jumbled assortment of public and private plans and wildly varying drug policies across jurisdictions is inefficient, costly and inequitable. But, above all, it says Canada pays too much for drugs – between 16 and 40 per cent more than other industrialized countries – in a bid to attract pharmaceutical investment. CBC
1 September
Health Minister accepts ‘prudent’ advice not to fund MS treatment
Vascular procedure to treat multiple sclerosis is invasive and too risky for clinical trials, Leona Aglukkaq says
Health agency dampens MS patients’ hopes by rejecting clinical trials
24 August
Keep Canadians in loop on health-care spending: A-G
Ottawa needs to do a better job telling Canadians how their health dollars are being spent and start making long-term projections to prepare for the aging population, auditor-general Sheila Fraser said.
Ms. Fraser also called on Tuesday for the federal government to undertake long-term fiscal projections to determine the challenges that lie ahead in funding the health-care system as the population ages. She also noted that Prime Minister Stephen Harper’s government should be projecting the long-term costs of climate change on the population.
Currently, the federal government only looks ahead about three to five years, said Ms. Fraser, and it should be looking down the road at least 25 years.
19 August
New MDs need choice, not coercion
(Gazette editorial) For years Quebec has used just one approach to the intractable problem of staffing hospitals and medical centres in far-flung regions: We force newly-minted doctors to move to places with which they have no connection, and in which they have no interest in setting up practice
… Across the U.S., almost 5,000 recent med-school graduates have accepted federal grants to pay off their school loans. The grants, averaging $150,000 per student, have a string attached: the young doctors must remain in rural or other under-served areas for three to five years.
3 August
CMA issues five-pillar plan for health-care reform
In a new report entitled “Health Care Transformation in Canada: Change that Works, Care that Lasts,” the CMA says health-care reform is urgently needed if the system is to remain sustainable in the future.
The report warns that many patients are unsatisfied with the level of care they receive across the system, and that Canadians are not getting value for dollars spent. The report cites the Euro-Canada Health Consumer Index, which ranked Canada 30th of 30 countries for value for money spent on health care.
The CMA’s so-called five pillars for transformation are:
* Refocusing the system so it serves the needs of patients. The report contains a charter for patient-centred care.
* Improving access to care and the quality of care, partly through funding incentives to health-care facilities that exhibit better efficiency and higher patient satisfaction.
* Identifying and correcting gaps in care, particularly the limited access to prescription drugs in some provinces and territories, and discrepancies in the delivery of services once a patient is discharged from hospital.
* Helping health-care providers care for their patients, be it through addressing staff shortages at facilities to adopting the most up-to-date health information technologies.
* Boosting accountability and responsibility at all levels in the system.
The report’s recommendations come after the CMA spent a year interviewing patients, policymakers and health-care professionals. (CBC) Help transform medicare, CMA tells Canadians
23 July
Harper, Aglukkaq singled out for stinging rebuke at AIDS conference
Julio Montaner, the outgoing president of the International AIDS Society who is also a Canadian, saved his parting shot for the government of Canada, issuing a sharp rebuke.
“I am ashamed to say that the Government of Canada has punched well below its weight in funding universal access and supporting those affected by HIV and AIDS in Canada and around the world.”
20 July
Ottawa’s AIDS strategy targets research, mother-child transmission
More than six months after its controversial decision to scrap a planned $88-million vaccine plant, Ottawa is renewing its partnership with the Gates Foundation in the fight against HIV and AIDS, this time pledging to redirect the unspent millions to research and to halting the spread of the disease between mother and child.
16 July
Shriners move ahead with Montreal hospital Finally some good news!
The $100-million hospital will be built on two hectares next door to the Montreal Children’s Hospital, part of the McGill University Health Centre in the city’s west end. It will replace the current hospital, an 85-year-old facility in dire need of repair on Cedar Avenue at the base of Mount Royal.
Thursday’s announcement came after a decade of delays, including a failed bid by the Ontario city of London in 2005 to move the facility there.
15 July
Quebec to create 500 ‘supernurse’ jobs -Nurse practitioners can provide primary health care
Nurse practitioners have a graduate degree and can prescribe medication and provide prenatal care. They are considered key to alleviating a shortage of primary health care in Quebec.
The 500 new nurses won’t be on the ground until 2018 because it takes time to train them: They need two years of field experience before earning their full practitioner title. [Ed. note: This actually means that all 500 won’t be in place before 2018; the first six have graduated from McGill, so presumably will be at work in two years.]
Quebec’s Health Ministry has been negotiating with physicians for years over bringing in more nurse practitioners. The GP federation has been reluctant, fearing doctors would lose money and patients. “The doctors want to have nurses in their practice, but with the condition that they don’t lose money,” Godin said. [There is something horribly wrong with this picture, when about 1/3 of Montrealers do not have a GP.] Quebec doctors in private practice will be eligible for a monthly $2,500 subsidy to take on a nurse practitioner. They will still receive their fee for service for every patient treated in their office, even if patients are seen by the nurse practitioner.
Press Release from the Federation of General Practitioners: La Fédération des médecins omnipraticiens du Québec (FMOQ) se réjouit de voir le gouvernement du Québec passer à l’action et annoncer des investissements importants qui permettront la création de 500 postes d’infirmières praticiennes spécialisées (IPS).
13 July
Quebec Medicare to cover in vitro costs starting in August
Health Minister Yves Bolduc announced Tuesday that fertility treatments for couples will be covered by Medicare as of Aug. 5, making Quebec the first place in North America to provide free in vitro fertilization treatments. It is estimated that the program will cost the government $25 million the first year, and up to $80 million by 2014. Not a universally popular decision. Given all the problems with current healthcare services, it seems there are many who feel the money would be better spent on other services. The Gazette editorial Unnecessary burden on our health system clearly expresses many legitimate concerns.
20 June
MUHC: Designing patient care
Sometimes, even the best-laid plans take a slight detour at the accounting office.
After years of wistful thinking and months of diligent consultation with everyone from the attending physician and front-line nurse to the folks who scrub the sinks, the McGill University Health Centre settled on a blueprint for the smart hospital room of the future.
Every adult patient would have a private room, a 25 square-metre space with a flat-screen television, art on the walls and a picture window looking out on the city, a children’s playground and the lush parkland below.
28 April
Wednesday Nighter Dr. Hing-Sang Hum replies:
Unfortunately, the health care system can’t claim all the credit. We have less gun shot injuries, less gang/drug trafffics, less war conflicts. we don’t supersize the steaks, fries etc.
Nature vs Nurture. we can’t choose our parents. But exercise regularly, eat sensibly with good sanitation probably goes a long way.
Canadians lead longer, healthier lives than Americans
Compared to their neighbours south of the border, Canadians live longer, healthier lives. Research published in BioMed Central’s open access journal Population Health Metrics has found this disparity between the two countries, suggesting that America’s lack of universal health care and lower levels of social and economic equality are to blame.
2 April
Superhospital sod turns – in a way
There will be no more delays in construction of the long-awaited McGill University Health Centre superhospital, the institution’s executive director said yesterday.
12 March
Hôpitaux en crise: les infirmières s’en prennent à Bolduc
La présidente de la FIQ affirme que la qualité des soins dans le réseau est directement liée aux conditions de travail des employés. Actuellement en négociation en vue du renouvellement de la convention collectives des infirmières, Mme Laurent accuse le gouvernement de faire preuve de «mauvaise foi»
11 March
Le directeur national des urgences démissionne
(La Presse) Alors que le réseau de la santé est en crise, le directeur national des urgences, le Dr Pierre Savard, quitte ses fonctions, a appris La Presse. Le cabinet du ministre de la Santé, Yves Bolduc, reste discret sur les raisons de ce départ et indique simplement que le Dr Savard souhaite «retourner à la pratique médicale».
Hospital crowding taking toll
(Montreal Gazette) ER horror stories; Maisonneuve-Rosemont patient dies in corridor
Figiel’s death, amid a lack of services because of overcrowding, is the latest in a string of recent emergency room fatalities that underscores a crisis in Quebec’s health care system.
The family had initially declined an autopsy.But Dr. Yoanna Skrobik, head of intensive care at Maisonneuve-Rosemont, alerted the family the next day that she had demanded an investigation into the death.
9 March
GPs lobby for raise
Earn 55% less than specialists; About 180 residencies remain unfilled in family medicine in last 3 years
(Montreal Gazette) As labour negotiations continue, Fédération head Louis Godin called a news conference to explain that 2010 will be “crucial” for the profession – and by extension, the patients. The federation is calling on the provincial Health Department to narrow the wage gap or suffer the consequences. According to data from the Régie de l’assurance maladie du Québec, the provincial insurance board, the gap keeps growing, from 20 per cent in 1975 to 55 per cent last year.
27 February
(Montreal Gazette) … overcrowding at Quebec’s hospital emergency rooms will be resolved in “four or five years.”
“We have the best health- care system in the world,” Health Minister Yves Bolduc said yesterday, while admitting patients sometimes have to wait for that care. “All the patients are well treated.” Bolduc said the situation has been improving across the province, but remains bad in Montreal and the city’s east end in particular. He said the critical situation at Maisonneuve-Rosemont hospital has been aggravated by an outbreak of gastroenteritis.
11 January
Experts waiting for Quebec to act on Alzheimer’s plan
Seven months after report was submitted, Health Department has yet to announce how it will proceed
Ignoring tomorrow, governing for today
(Ottawa Citizen) The Alzheimer Society has released its report as a call to action, citing the progressive moves made by other countries and challenging governments here to do the same. But in this Canada of 2010, led by a federal government that can’t see beyond the pragmatic expediencies of its own re-election, don’t count on anything happening.
The reason is simple. Government action generally means government spending. And government spending, in the Stephen Harper regime, generally means directing dollars to a narrow ideological agenda and to immediate vote-winning areas. The terrible outcomes predicted in Rising Tide are too far off to be politically engaging now.
In Canada these days, we live in a time of small, cribbed minds. Of goals that extend no farther than the next election. Of short-sighted decision-makers and visionless leaders.
4 January
Dementia will take huge toll as boomers age
(National Post) A new study by the Alzheimer Society of Canada says the country urgently needs a strategy to minimize the impact of the baby boomers’ march toward dementia.
The study, Rising Tide: The Impact of Dementia on Canadian Society, suggests that 1.1 million Canadians will have Alzheimer’s disease, or a related dementia, by 2038.
If not mitigated, dementia’s prevalence will create a tenfold increase in the demand for long-term care beds and cost the Canadian economy a staggering $97-billion annually, the study found.
2009
30 December
The top 10 Canadian health news stories of 2009;
Medical marijuana
Marijuana’s journey to legal health treatment: the Canadian experience
Some users complain about the quality of the federal cannabis or say they need a different strain of pot than the single standardized one produced by PPS. As a result, many choose to grow their own or head to the black market.
Activists have long wanted Ottawa to loosen the rules that prevent providers (other than PPS) from supplying more than one patient. New rules were implemented in 2009 to allow designated producers to grow marijuana for one additional approved user — to a maximum of two. But that fell far short of what many in the community had wanted.
Eight years into the adoption of the Marijuana Medical Access Regulations, many activists remain frustrated with the bureaucracy and the limitations. Ottawa has shown little enthusiasm for further loosening the legal restrictions on a drug that it says still deserves a tight leash.
15 December
UBC plans to test potentially groundbreaking MS treatment
(Globe & Mail) The University of British Columbia has announced plans to begin patient trials to test a potentially groundbreaking method of diagnosing and treating multiple sclerosis. It’s the first research proposal in Canada to suggest evaluating the findings of Italian doctor Paolo Zamboni whose early studies indicate that multiple sclerosis might be caused by vein blockages that lead to a buildup of iron in the brain. Researcher’s labour of love leads to MS breakthrough
13 December
A Breath of Fresh Air for Health Care
Even the most seemingly innocuous details — a dead potted plant in a reception room, an ill-fitting hospital gown, a blaring television — can contribute to an unpleasant experience.
One Wednesday Nighter with long experience in Health care commented on this article: Kaiser Permanente is well known, has been in existence a long time, as have many similar institutions. I am in total agreement that most hospitals are very poorly designed if their goal is to achieve what is best for the patient. For starters, I believe that it is inhuman to jam a sick person into a multiple bed unit and indeed, the newer establishments are designed to maximize privacy. In the twenties and thirties when very little could be done for patients, it made sense to have large ward where the Nurse could move those most ill closest to the nursing station and patients were of help to each others, but this is the twenty-first century (I believe). The closest that I have seen to the ideal, unfortunately, is a palliative care facility in Pointe Claire. The calm and breathing space enables those at the end of their life to die in the presence of their friends and family, in a very agreeable ambiance.
11 December
Getting it online: The emergence of the e-patient
Getting health information online.Your child’s under the weather. You’re certain the little tyke’s running a fever. You’re not sure what to do, so you turn to the internet and find some tips from a source you figure you can trust, like the world-renowned Hospital for Sick Children in Toronto. You follow those tips and instead of adding to the lineup in the emergency department, you deal with the problem at home and save the health-care system a little money.
9 December
Superhospital’s cost might double
Projected at $800M in the 1990s; MUHC dismisses report of soaring price tag as rumour
2 December
More family doctors needed in Canada, report urges
(CTV) Canada should aim to ensure 95 per cent of people in every community have a family doctor by 2012, urge the Canadian Medical Association and the College of Family Physicians of Canada.
The groups, which banded together two years ago to form the Primary Care Wait Time Partnership, say in order to reach this target, the country needs to increase the number of family doctors practising in Canada while also increasing the capacity of existing family physicians.
In a report released Wednesday, entitled “The Wait Starts Here”, the groups note that reports on wait times have focused mainly on access to specialty care, such as MRI diagnostics. But attention also needs to be paid to the ongoing problem of a shortage of family doctors, they say.
21 November
Henry Aubin: Abandon the PPPs
It’s not too late to return to the traditional way of building hospitals
(Under a PPP, a consortium would finance, design and construct each hospital, then maintain it for 30-odd years. Under the conventional mode, Quebec would design and maintain the building, leaving it to the private sector only to construct it).
Policy Options November 2009
“Canadians overwhelmingly support universal health care; think Obama is on right track in United States” by Nik Nanos
Nine Canadians out of ten support the principle of universal health care with a single insurer — the government. The principle of universality is itself the most popular feature of the public health care system, while waiting times are identified by a wide margin as the biggest problem. Seven Canadians out of ten also think Barack Obama is on the right track with his health care reform proposals in the United States. Contributing Writer Nik Nanos reports on the findings of his latest exclusive poll for Policy Options.
16 November
Medical establishment prevents nurses from assuming new roles
Study published in Recherches Sociographiques by University of Montreal researchers
Montreal, November 16, 2009 – Physicians still retain the bulk of decision-making power over nurses in Quebec – a situation that’s detrimental to evolving nursing roles. According to a new study by Université de Montréal researchers, published in Recherches Sociographiques, nursing functions are still very much assigned by physicians who often oversee family medicine groups (FMGs), specialized nurse practitioners (SNP) and oncology nurse navigators (ONN).
7 October
(WN #1440) Quebec has the dubious distinction of being the province with the greatest shortage of full-time family physicians – roughly 25% of the total population, and 34% of Montrealers, do not have access to a family doctor. The shortage is now estimated at 1,105. There are encouraging increases in numbers of graduating students (from 150 should reach 300 next year), but simply to maintain the current level (shortage) there is a need for an annual average of 350 new family doctors starting practice, which may be hard to achieve when eight percent of Quebec graduates leave.
9 September
First of new health-care clinics launched in Quebec – will most probably not achieve the desired results because the planning will be done centrally and the biggest problem facing Quebec is the dearth of family physicians (the shortage is estimated at 700). The definition of means rather than results is dependent on only the intellectual capacity of the planners to the exclusion of those on the front line. This appears to be slowly being recognized by some in the school system.
30 June
Quebec spends $100 million on nurse incentives
Health Minister Yves Bolduc said the government would offer graduating nurses an annual bonus of $3,000 for the next three years if they commit to work a certain number of hours in the public health-care sector. Graduating nurse practitioners would receive $2,000 and experienced nurses who agree to delay their retirement would receive an annual bonus of $8,000 over three years.
14 May
Canada to United States of America nurse migration
Nursing study published today in the International Nursing Review concludes it’s not just about the money
A study looking at Canadian-educated registered nurses working in the USA found that opportunities for ongoing education, including formal support for graduate education and ease of licensure, in addition to full-time employment, were key factors that contribute to the migration of Canadian nurses to the USA, particularly baccalaureate-educated nurses.
22 August 2006
(CBC) Canada Health care
One Supreme Court decision may have done more to change health care in Canada than three major reports and a first ministers conference that ended with a $41-billion infusion into the system.
On June 9, 2005, the high court struck down a Quebec law that prohibited people from buying private health insurance to cover procedures already offered by the public system.


